Abstract
Introduction
Follicular lymphoma (FL) is characterised by a vast clinical and molecular heterogeneity. Whereas early progression of disease (POD) within 24 months has been identified as an important prognostic factor in different cohorts, potential associations with number of treatment lines, treatment sequencing and survival have not been thoroughly described in real world data. To further identify patient groups with a high need for novel therapeutic strategies in clinical routine and for inclusion in clinical trials we aimed to describe treatment patterns and survival in a national population-based setting.
Methods
We identified all patients diagnosed with FL in the nationwide Swedish Lymphoma register (coverage >95%) during the period 2007 to 2014, with follow-up through 2020. Information on progression, relapse, transformation and treatments was collected through review of medical records. A total of 2,079 patients were identified. Patients who did not provide informed consent (n=40), were diagnosed with transformed FL (n=144) or grade 3B (n=72), or where medical record data was missing (n=51) were excluded. The main analysis included patients receiving any first-line systemic treatment. Patients who were initially managed with radiotherapy (RT) only or a watch and wait (WaW)-approach were included in the main analysis if/when they received their first systemic treatment. Consolidation treatment including RT, maintenance with anti-CD20 antibody therapy or autologous stem cell transplantation (ASCT) was noted but did not count as separate treatment lines. Overall survival (OS) was illustrated graphically with the Kaplan-Meier method.
Results
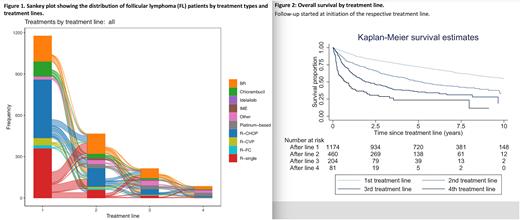
In the final cohort of patients with FL (N=1,772), median age at diagnosis was 65 (18-98) years, and median follow-up time was 6.7 (0.003-13.9) years. Overall, 412 patients (23%) were managed with WaW only during the entire follow-up. Among patients with stage I or limited stage II disease treated curatively with RT at diagnosis (n=304), 60% (n=181) never needed additional therapy. In total, 1,174 patients (66%) received any first systemic treatment. The most common first-line treatment was R-CHOP (425/1,174, 36%), followed by R-single (361, 31%) and BR (184, 16%). The use of R-CHOP as first-line treatment decreased between calendar periods, whereas the use of BR and R-single in first line increased. Among patients starting any first line, 460 (39%) received systemic second-line treatment. Here, BR was most commonly administered (143/460, 31%) followed by R-CHOP (136/460, 30%) and R-single (60/460, 13%). A third-line treatment was administered to 204 patients (17%). Again, BR was most commonly chosen (67, 31%), followed by R-CHOP (41, 19%) and platinum-based chemotherapy (28, 13%). Only 81 (7%) patients required fourth-line treatment, and the maximum number of treatment lines administered were seven. The number of patients treated with the varying regimens in first and subsequent treatment lines are presented as a Sankey plot in Figure 1.
Time to next treatment decreased with increasing number of treatment lines, as did OS. Time to next treatment was 2 years on average from the first to second treatment lines, 1.4 years to third line and 1 year to fourth line. The 5-year OS from first-line treatment was 75%, and the corresponding figures following second, third and fourth lines of therapy were 53%, 36% and 24%, respectively (Figure 2). During the whole study period, 173 (15%) patients received systemic treatment due to transformation, 258 (22%) received R-maintenance and 79 (7%) patients underwent ASCT.
Conclusion
In this national population-based cohort of FL, one in four patients never needed active oncological treatment. Among patients starting any first-line systemic therapy, 39% required a second line, and 18% a third line over a median follow-up of about 7 years. Further, time to next treatment decreased with increasing number of treatment lines and number of treatment lines was associated with dramatically worse survival. We conclude that, in addition to patients with FL experiencing POD24, patients who require multiple treatment lines (≥3) constitute a group with a large clinical unmet need, and methods to identify these patients at an early stage are warranted. The present results provide valuable real-world reference data for the design and interpretation of clinical trials of new treatments in FL.
Disclosures
Weibull:War On Cancer: Current Employment; Janseen Cilag: Research Funding; Red Door Analytics: Membership on an entity's Board of Directors or advisory committees. Wahlin:Roche: Consultancy, Research Funding; Gilead Sciences: Research Funding. Andersson:AbbVie: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Gilead: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; AstraZeneca: Speakers Bureau; Janssen: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Roche: Speakers Bureau; Beigene: Membership on an entity's Board of Directors or advisory committees; Takeda: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Ekstroem Smedby:Janseen Cilag: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal